Article
Three challenges with an outsized effect on rural hospitals
Healthcare is an extremely complex industry that is always evolving, from scientific breakthroughs and emerging diseases to payment reform and new technologies. Hospitals across a variety of settings share many of the same challenges keeping up with these changes and managing ongoing demands. However, the way these issues affect rural hospitals can differ given the unique needs and characteristics of these organizations and the communities they serve.
Here are some of the top issues rural hospitals are currently dealing with:
Remaining financially solvent and independent
Financial strains on rural healthcare organizations are not new, but many are now coming to a head, especially in the wake of the COVID-19 pandemic. The Center for Healthcare Quality and Payment Reform estimates that approximately one-third of rural hospitals are at risk of closure, and it classifies 200 of those 600 at immediate risk of closure. Research published in Health Affairs also reveals that over an eight-year period, 17% of unprofitable rural hospitals were merged with other organizations, oftentimes with organizations that are not local to their own region.
Moreover, Medicare payments were cut by 2% in 2023, and will fall at least another 1.25% in 2024. Given that rural hospitals often serve a higher proportion of Medicare beneficiaries, even a small reduction in payments can have a noticeable impact.
 Maintaining adequate staffing levels
Maintaining adequate staffing levels
The wave of job changes and early retirements stemming from the pandemic deepened the ongoing staffing problem, and rural hospitals already often face more significant hiring challenges than their urban and suburban counterparts. For example, they must attract specialists to communities where there may be fewer resources to work with. Additionally, this year, there are hundreds of unfilled emergency department residency positions, and patients in rural settings often rely on the ED if other healthcare facilities are dozens, if not hundreds, of miles away.
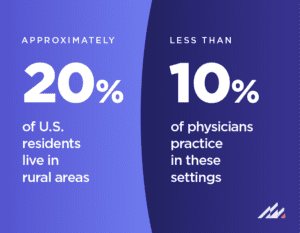
While approximately 20% of U.S. residents live in rural areas, less than 10% of physicians practice in these settings. Given how widespread staffing shortages are, small hospitals are competing with large health systems to tap into the talent pool. This may mean a heavier reliance on hiring contractors to fill staffing gaps, which typically are more costly to organizations, further compounding budgetary constraints.
 Managing health information technology
Managing health information technology
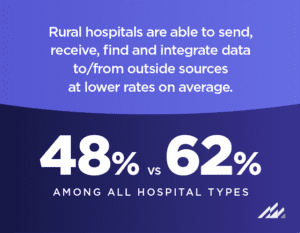
Financial burdens and staffing hurdles are intertwined with a third challenge rural organizations are contending with: technology management. Organizations want to get the most out of their health IT, but it is difficult to maintain and upgrade complex systems when your IT staff members are spread thin. Additionally, rural hospitals are able to send, receive, find and integrate data to/from outside sources at lower rates on average (48% versus 62% among all hospital types), adding to the load of clinical and non-clinical staff. And, rural hospitals often struggle to hire cybersecurity professionals, which makes it more difficult to protect against, monitor for and respond to security incidents.
Members of Congress have introduced the Rural Hospital Cybersecurity Enhancement Act, which would help create a workforce development strategy to address cybersecurity gaps, if passed. There are additional strategies rural hospitals can choose to mitigate cybersecurity and broader IT challenges. Opting for an electronic health record (EHR) system that is designed with industry standards in mind and that simplifies data management can help, as well as leveraging a system that integrates ambulatory and acute records. Additionally, hosting in the cloud through an EHR partner can offload network and infrastructure responsibilities, enable hospital staff members to focus more on day-to-day tasks and give under-resourced organizations more affordable access to advanced security controls.
Altera Digital Health understands rural hospitals are juggling many challenges—and for 25 years, Paragon® has supported these critically important organizations’ health IT needs. Learn more about Paragon here.