Finding your financial footing
In healthcare, challenges are to be expected. But overcoming them shouldn’t overburden your people or your bottom line. That’s why we do what we do.
You don’t have the time or energy to stay current with every regulatory requirement or where to find every data point you need. Together, the path toward your organization’s financial peak is laid out, and step-by-step, we’ll get there. That’s why we’re here.
We make value-focused initiatives easier to design and implement by giving you solutions at every step that make accessing and connecting with the insights you need to improve reimbursements and drive down the cost of care. Without sacrificing the quality.
In fact, our claim-based submission and denial management support alone can save a 100-bed hospital as much as $11.4M.
Altera experts identified the following three specific areas that, when addressed accordingly, will help you achieve better financial stability:
Streamlining bottom lines
Finding the right tools
The contracts healthcare organizations have with payers change only so often (i.e., annually). At the same time, the cost of care has gone up amid inflation and cost increases for medical supplies and pharmacy and drug charges. This means organizations must find ways to reduce their operating expenses to improve margins between contract negotiations. And identifying the financial levers to pull begins with having the right data.
When assessing current or potential revenue cycle solutions, financial leaders should look for those that provide visibility into meaningful metrics, such as:
Getting a monthly summary of these numbers (if not daily for DNFB and DNFC) can point leaders to potential issues to investigate. When drilling down into these metrics at a more granular level, leaders can then find the low-hanging fruit to improve the speed and accuracy of claims getting out the door so they are submitted properly the first time and the maximum reimbursement is received sooner. This also enables staff members to identify any patterns among denials so they can add touchpoints upstream in the revenue cycle, address their root causes and ultimately drive down A/R days.
In addition to leveraging the right tools, healthcare organizations need the right people to achieve optimal financial performance. For some, that might mean bringing in a third party that can find and help remedy your internal team’s blind spots, such as Altera’s Revenue Cycle Center of Excellence (RCCOE).
The COVID-19 pandemic has shaken up the healthcare workforce, and that includes non-clinical yet essential roles, like those in registration and financial counselors, that already had high turnover rates. Having an external partner examine your organization’s productivity metrics can help identify high performers and the best way to delegate tasks, particularly those with the biggest influence on finances.
An external partner can also conduct a workflow assessment to uncover opportunities to bring greater efficiency to your revenue cycle management processes so you can minimize the pressure on the staff members you do have. This may be particularly helpful to see if there is any misalignment between your workflows and any regulatory changes that have occurred since those were established.
Additionally, a third party can assist your team with vendor management to ensure your contracts are being honored. For example, there may be a payer that is acknowledging or denying pay within 90 days when you actually negotiated 30 days. Holding payers accountable in this way can help speed up cash flow, and any improvement can go a long way when operating on thin margins.
Sharing knowledge, connecting workflows—in real time
It’s a simple concept: when everything you need is in one place, it’s easier to achieve impactful results. The same applies to the information driving your organization. When you have a dashboard displaying all the relevant information in one place, it’s simpler to make decisions that will have a positive result. However, as we know, healthcare is an extremely complex industry filled with regulations that affect more than just claims and reimbursements. This is why there’s immense importance to how you’re keeping track of this information and how that solution is streamlining information to be as simple as possible, while also eliminating duplicative steps.
This underlines the importance of having a credible dashboard that can display how your organization is performing compared to the rest of the industry and what’s needed to improve. Its background should be tied into HFMA standards, for example, and be able to display trends over time to give the most holistic view possible of relevant metrics and data. To be relevant, this dashboard also needs to be on the pulse of changing regulations.
The healthcare delivery system requires a single source of truth, where data has been integrated and structured in a framework engineered for key performance indicator (KPI) development and dashboard construction. These KPIs, such as days in A/R, DNFB and denial tracking are at the heartbeat of any organization. Your dashboard solution should include a comprehensive toolkit focused on identifying electronic health record (EHR) utilization and opportunities. Users should be able to easily configure quality measures to support quality initiatives. From there, measure dashboards and scorecards should be automatically triggered and available to support analysis of organizations’ initiatives so they can drill down on the intricacies of a potential problem or non-compliance.
Dashboards can be powerful tools, used to enable organizations to reach new heights. If your organization needs a new dashboard solution, learn more here.
Accelerating reimbursements
Positioning yourself for a better journey through changing needs and regulations
As much as healthcare organizations must focus on their communities, they also must keep the lights on and continue to make investments back into themselves. Financial stability is a pillar of what keeps an organization healthy, which is why in the near future, and after disruptors such as the COVID-19 pandemic, it’s more important than ever for healthcare organizations to reclaim their financial health.
Therefore, the importance of introducing efficient tools to enable your organization to reach new heights is now more relevant than ever. Consider leveraging robotic processing automation (RPA), a software bot developed using AI and machine learning (ML) that replicates actions and workflows normally performed by a human, enabling greater productivity and efficiency. This technology is often applied to highly repetitive, tedious work, making it well-suited to lower-value tasks within the billing office. While a person may take several minutes to complete a task, a bot can perform the same action within seconds. RPA uses historical claim data to identify claims that are at risk for denial and alert your office staff. This gives staff members an opportunity to correct claims before they are submitted, thus saving time that would be spent correcting and resubmitting claims—and decreasing the time to receive reimbursement.
As the RPA “learns” over time, it can suggest actions to correct claims, further reducing time staff members spend on manual efforts. Rules can also be applied to the bot so it can automatically correct claims based on repetitive processes and learnings, removing the need for manual intervention altogether. Now your office staff is available to work with the more complex cases that RPA can’t handle.
However, RPA is not a universal revenue cycle management (RCM) fix for every organization. RPA must be tailored to address the needs and challenges of each organization, so an assessment of RCM processes must be made to ensure that this investment is being made in the right places. Staff training and support must also be considered to reduce time spent adapting to the new solution.
Overall, RPA is a valuable tool that holds great potential to reduce costly RCM processes within the right organization. As a leading provider of healthcare technology solutions, Altera has the expertise needed for assessment and discussion. As we look toward the future, we’ll keep driving forward with RPA technology, which we’ll discuss more soon.
Better communication leads to cleaner financial operations
Many of the difficult challenges in the healthcare revenue cycle result in duplicative work, lost charges and wasted time for staff. All of this results in time that could be better spent in other areas. To bring forth next-level healthcare, we strive to help our clients better use the time they do have. With that in mind, here are some of the primary (and avoidable) mistakes many organizations make in their approach to billing.
Failing to conduct eligibility checks up front. Staff members should confirm patient identity and payer information before any charges are incurred. Billing the wrong patient or the wrong payer creates substantial rework on the backend and delays when organizations can receive payment.
Entering charges separately from orders. Charges should generate automatically in the billing system based on orders as they are being written within the EHR. . Not only does this save your team from duplicating work, but it helps prevent late and missed charges.
Manually calculating the number of supplies used on a patient. Record the exact number of supplies used during a patient visit or procedure by using barcode scanners. These scanners should also connect to your billing system so that patients and payers are properly charged for the correct number of supplies.
Allowing lingering charges to delay the billing cycle. If your billing solution is unable to capture charges as they are incurred, your organization may have extended wait times before it can issue a bill. The sooner a bill is issued, the sooner your organization can get paid.
Neglecting to analyze denied claims. You should have access to a regular statistical analysis of your billing department. This can help you pinpoint potential areas of concern and prevent your team from repeating commonly made mistakes that lead to denials.
Denying denials: Staying ahead when it matters most
One of the keys to maintaining financial stability in any healthcare organization is minimizing denials. Denials can happen for many reasons, but here are the top three reasons a claim may be denied and what your organization can do to minimize the risk:
You’re billing the wrong patient. Health systems often use a variety of IT solutions throughout their organizations to meet the unique needs of each department. But this can lead to miscommunication between your EHR and revenue cycle solution if you have multiple patients with the same name. To avoid this, organizations can use what is known as an Enterprise Master Person Index. This type of solution assigns a unique identifier to each patient that acts as a “glue” between disparate systems within your organization and ensures that the correct patient is billed.

You’re failing to complete medical necessity checks. To comply with Medicare and receive payment, organizations must complete medical necessity checks on all outpatient procedures. If a procedure won’t be covered by Medicare, then you need to secure an advanced beneficiary notification signed by the patient before any services are rendered. Failure to do so leaves your organization responsible for all costs incurred for that particular procedure. Consider a solution that can automate medical necessity checks by integrating with your EHR and revenue cycle solution. It should also automatically update on a regular basis to make sure your organization is in compliance with any changes from local or national governing bodies.

You don’t have standardized coding. Many organizations have developed a “homegrown” approach to the way they code charges into the system. This can be a largely subjective method, meaning that costs could be coded differently depending on who is recording them. This is particularly a problem in outpatient settings, such as the emergency department, where a patient may require a number of injections or infusions, which tend to be complicated to code. Discrepancies in the coding can lead to missed charges or denials from payers. To avoid this, organizations should consider implementing a solution capable of automating the assignment of coding hierarchy for the entire patient visit based on current CMS and CPT guidelines.
Unburdening your people
What’s really at risk within data-sharing shortfalls
You wouldn’t expect electricians or firefighters to perform their jobs without the right equipment. But in healthcare, providers often must deliver the best care possible while missing a crucial tool: patient data.
This largely occurs due to a lack of interoperability among different health IT solutions. And according to HIMSS Analytics, the average hospital has as many as 16 EHR platforms in use at affiliated practices. Here are a couple reasons healthcare leaders need to identify and fix data-sharing shortfalls within their organizations to improve clinical decision-making—and financial performance.
Care experience consequences
When organizations have poor interoperability, clinicians often have to switch back and forth between multiple systems to find the information they need. Considering how many patients a single provider might see in a day, this unnecessary waste can really eat up time and slow patient throughput. When clinical data is disorganized or missing altogether from the patient record, clinicians may also unknowingly order duplicative tests that are costly to the organization.
Additionally, clinician burnout has been an issue for several years now, and interoperability challenges only make matters worse. While it is difficult to calculate the exact cost of data-sharing shortfalls, organizations are cutting into their budgets to retain staff and hire amid the healthcare workforce shortage. Improving interoperability is one step organizations can take to relieve some of the technology hurdles effecting provider experiences and wellbeing. U.S. Surgeon General Vivek Murthy MD, MBA, recognized the issue in an advisory on provider burnout, saying, "Technology companies can ensure that patient-generated data is accessible in a meaningful way and does not result in increased burdens on health workers . . . This includes improvements in interoperability to optimize communication between and across disparate systems and sources, such as care teams, laboratories and public health."
Regulatory requirement readiness
Provider organizations in the U.S. also now need to meet the information-blocking requirements coming out of the 21st Century Cures Act or they risk being fined for non-compliance. This means organizations must be able to share electronic health information (EHI) with other “actors” (i.e., hospitals, pharmacies, health information exchanges) without interference.
Aside from avoiding penalties, there are also regulatory incentives for provider organizations to improve their data-sharing capabilities. In 2022, the Centers for Medicare & Medicaid Services (CMS) finalized changes to the Medicare Promoting Interoperability Program for eligible hospitals and critical access hospitals (CAHs) attesting to CMS. This program rewards organizations that meet specific interoperability-related measures through increased reimbursement.
Automating what takes your people away from where they really count
The claim-denial process is often a weak spot in the revenue cycle. However, that means there is massive opportunity for improvement. According to one study, the typical time spent processing acute patient claims ranges from 4.22 minutes for a general inpatient visit to 45.55 minutes for an inpatient surgical visit. If there are issues with data completeness or accuracy that lead to a denial, the time spent reviewing, correcting and re-submitting a claim can delay the processing of that claim for 12 to 48 hours. The longer a claim takes to process, the longer your organization must wait before you can receive payment. Additionally, your staff is spending its time resubmitting the same claim over and over again, instead of moving on to other claims and tasks.
There are a couple of ways to alleviate the burden placed on your staff during this process. First, as mentioned above, is using RPA. RPA can automatically correct claims based on what it’s learned and can complete highly repetitive tasks in a few seconds, whereas the same task may take several minutes if done manually. Now your staff is available to work on more complex tasks instead of being bogged down by tedious work.
Second, improve workflows wherever you can to improve productivity. For example, think about how many applications and solutions your organization uses. Now imagine how much time your staff members may spend searching for the right patient across that multitude of solutions as they navigate between them. And if the wrong patient information is inadvertently used during the billing cycle, your payment is denied, and now your staff has to spend time correcting the issue. Instead, use a solution that’s capable of synchronizing patient files across multiple applications. This way, when a clinician or staff member selects a patient in one system, all applications automatically open to that patient’s data, and any newly launched applications instantly navigate to that same patient, too. By streamlining access to patient data, you can reduce unnecessary cognitive burdens, increase productivity and support positive patient identification, which, in turn, leads to safer healthcare for patients and more accurate billing for your organization.
Giving your people more to work with by quieting the noise
People are at the heart of any organization, but in healthcare, people are both the drivers of the care and the ultimate result: receiving it. In order to enable care for both communities and individuals, healthcare organizations must be healthy themselves, albeit financially. There’s a lot that goes into financial health, but a driver that isn’t always obvious is giving your clinicians the right tools, the first time around, and the impact that has on the organization as a whole.
We know that EHRs have a great deal of importance for an organization. They are solutions that are used every day and can make or break a clinician’s (or even patient’s) ultimate experience. It’s no secret that these tools can often be cumbersome and add to the overall stress and misunderstanding that can spur negative results. At Altera, we know this, and in response, we are utilizing the methodology of Human-Centered Design (HCD) to create solutions that are more intuitive. In this process, our Human Experience (HX) team sits down with clinicians to collaborate on solutions that can work for any organization. Assisting our designers in this process gives clinicians a clear voice in the product. Since the initial investment is in the solution that was designed to work intuitively with clinicians, you’re not needlessly spending money down the road to fix something that doesn’t work for your organization.
The snowball effect of having the right solution, the first time around, is immense. Clinicians experience less burnout, which leads to a reduction in stress and less turnover. They’re able to work more efficiently, and these impacts create an overall better financial outlook. There’s no need for the expense of getting something fixed or added when the first solution covers all the necessary bases. Financial stability is a balancing act, and having the right solution can give your organization the stability it needs to drive positive change.
If you’d like to learn more about how we’re developing the right solutions that can fit your organization’s needs, download our Field Guide.
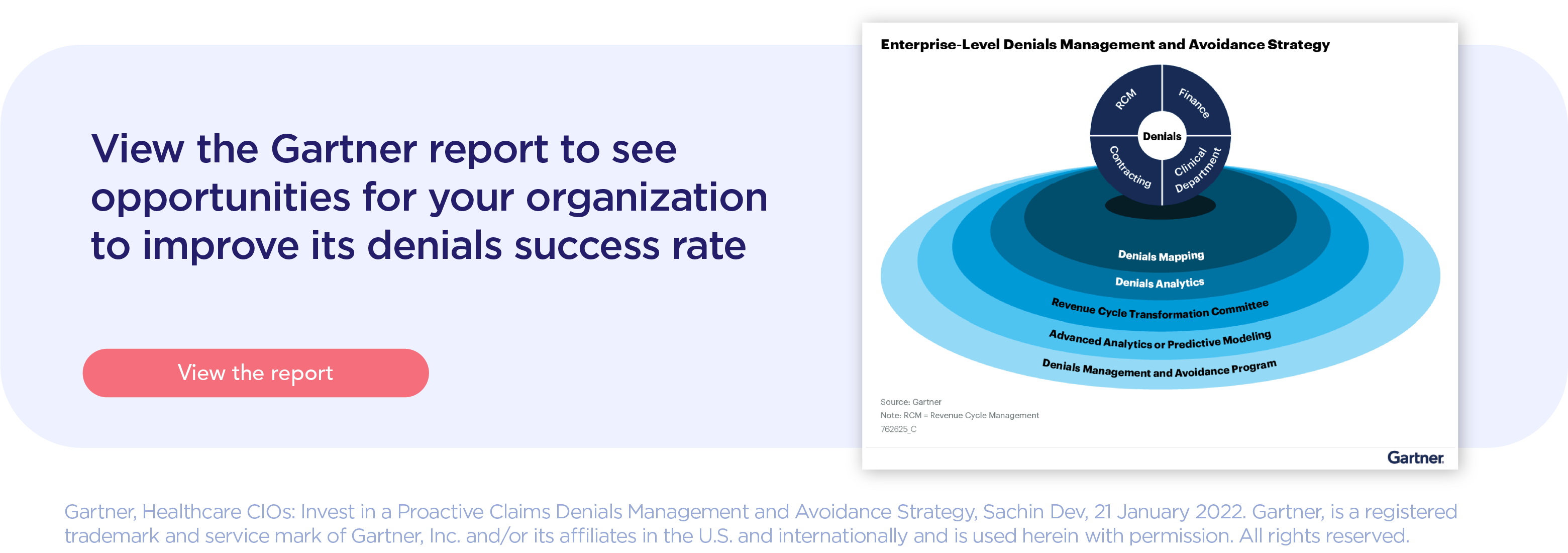
Gartner® report: Healthcare CIOs: Invest in a Proactive Claims Denials Management and Avoidance Strategy
According to a 2022 Gartner report, U.S. healthcare providers are facing mounting operational costs and revenue risk due to preventable, high-cost claims denials. At Altera, we agree with this report and second the advice that healthcare CIOs must morph their RCM technology with predictive insights and hyperautomation to improve their success rate of denials. In support of this detailed report, Altera experts and solutions work with your organization to build upon your financial foundations, one step at a time.
In this report, you’ll get a deeper look in the following key findings:
- "Healthcare delivery organizations (HDOs) rework as many as 20% of claims submitted to payers, which not only increases the operational cost of managing denials but also increases financial risk and adversely impacts profitability."
- "Simultaneously, HDOs are writing off millions of dollars in uncompensated care due to payer claims denials. HDO CIOs continue to struggle to find an effective IT solution blueprint to gain visibility into their payers’ denials trends."
- "HDO CIOs often conflate the concepts of denials management and denials prevention, leading to suboptimal financial performance. Additionally, revenue cycle leaders rely mainly on canned denials reports and lack descriptive and predictive analytics to proactively address denials or tackle underlying issues upstream in the revenue cycle management (RCM) process."
Access the whole report here.
Let’s connect
Discover how we can partner with you and, together, ascend to new heights in healthcare delivery.
Insights
Learn from thought leaders and industry experts on today’s most pressing healthcare topics, including value-based care, interoperability, reimbursements, genomics, and more.