Article
Patient identification and safety: The truth can be scary
Did you know that the Emergency Care Research Institute (ECRI) named patient misidentification one of the top 10 threats to patient safety? Related to that staggering stat is that patient identification was also outlined as a top priority of the American Health Information Management Association in its 2023 letter to Congress. I’ve written in the past about the dangers of disparate systems in healthcare, but in honor of Patient Safety Awareness Week I’d like to revisit the topic with an emphasis on the impact to patients.
Your identity matters (even more than you think)
Consider this scenario: A patient with severe kidney disease has a simple procedure performed on his foot. The patient assumes his medical records are being shared with and accessed by his doctors, so he does not mention his kidney disease to his podiatrist. However, the podiatrist’s records are separate from the nephrologist’s, so they are unaware of the condition and prescribe an antibiotic that can affect kidney function or even cause kidney damage.
The Emergency Care Research Institute (ECRI) named patient misidentification one of the top 10 threats to patient safety.
Now consider this scenario: A woman is suffering from two severe medical conditions that require her to see multiple specialty doctors within the same hospital system. Each doctor’s office has inadvertently created the patient’s individual record, as a result creating a duplicate patient record within the system. By creating two records for the same patient, they are unaware of medications that have been prescribed by each individual physician. Eventually the woman begins to experience new symptoms, including a fatigue so severe that she cannot function in everyday life. A trip to another specialist reveals that she has been overmedicated by the other doctors who were unknowingly prescribing similar medications.
Do these scenarios seem outlandish to you? They shouldn’t. They’re based on real-life experiences I’ve heard from some of my colleagues over the years. Think about your own medical history and prescriptions. What could happen if your doctor was missing a critical piece—something you assumed they would know? Or, in a terrible scenario, perhaps you become incapacitated and unable to share vital information about your health. What then?
Even more concerning, the inability to share information between organizations and providers isn’t the only way that disparate systems leave patients vulnerable to adverse outcomes. Wrong-patient errors, in which one patient’s record contains information mixed with another patient’s information, and duplicate patient errors, where a single patient’s information is associated with more than one matchable entity, are also threats to patient safety.
What can we do?
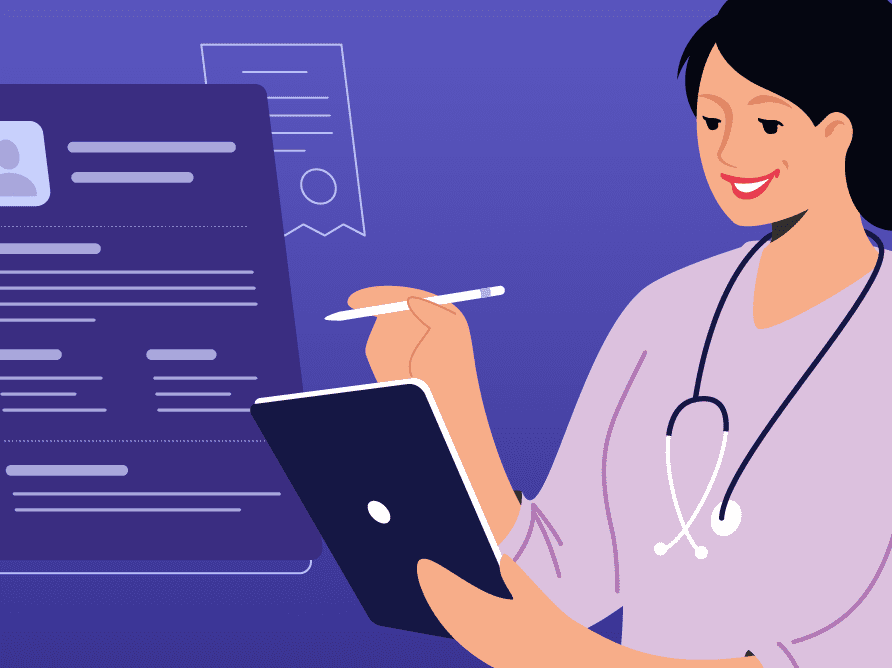
In all of these scenarios, allergies can be missed, adverse drug interactions can be missed, redundant tests could be performed (leading to a delay in diagnosis and treatment) and so much more. And the truth is, we can’t rely on manual labor to clean up duplicate records or prevent their creation in the first place. Most duplicate records are created during the registration and scheduling process, particularly in the Emergency Department where staff simply don’t have the time to comb through multiple records every time they need to admit a patient. As for cleaning up those duplicates, consider this: The average organization has a 23% duplicate rate and it takes approximately 15 minutes to clean up each duplicate. To put that into perspective, a 25-bed hospital has approximately 130,000 records, meaning about 30,000 of those records are duplicates.
To protect their patients from these risks, organizations need to consider implementing an Enterprise Master Patient Index system, or, EMPI. EMPIs use a unique patient identifier that acts as a “glue” between disparate systems within an organization, ensuring the correct patient file is used. EMPIs promote accurate identification across all solutions while maintaining data integrity, improve an organization’s interoperability and serve as a message broker between systems. One survey found that hospitals without an EMPI averaged a 17% match rate between a patient and the correct record vs a 94% match rate at hospitals with an EMPI.
Of course, there are many other benefits to using an EMPI, so this won’t be the last time you hear from me on this topic. But I would argue that better patient safety is the most important benefit to any healthcare IT solution. Afterall, striving for better and safer patient care is why we do what we do.
If you’d like to learn more about Altera’s EMPI solution, go here.