Article
Battling the opioid crisis: An update on the epidemic
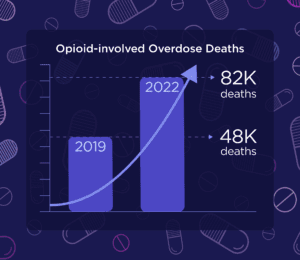
While the opioid epidemic may have faded from the media during the height of the COVID-19 pandemic, it certainly didn’t disappear from the lives of so many. In fact, the crisis has been quietly growing and is only recently making its way back into the spotlight. To recap, there were nearly 48,000 opioid-involved overdose deaths reported in the U.S. in 2019. Current data predicts that that number rose to 82,998 deaths in 2022. While providers and advocacy groups have certainly been staying on top of the crisis, it’s important for every person in the healthcare ecosystem (including healthcare IT) to understand and stay informed on this issue. Here are the latest updates:
Combining fentanyl and stimulants is creating a “fourth wave.”
According to a study recently published in Addiction, overdoses involving both stimulants (such as cocaine or methamphetamine) and fentanyl accounted for 32% of U.S. overdoses in 2021 and nearly 35,000 deaths. (For reference, polysubstance overdoses involving fentanyl and stimulants only accounted for 0.6% of overdose deaths in 2010.) The article posits that this indicates a shift into a “fourth wave” of the opioid crisis, which began with the first wave in the late 1990s or early 2000s and consisted of a rise in deaths related to prescription opioids. The second wave began in 2010 as heroin-related deaths increased and the third wave is said to have begun in 2013 with an uptick in illicit fentanyl use.
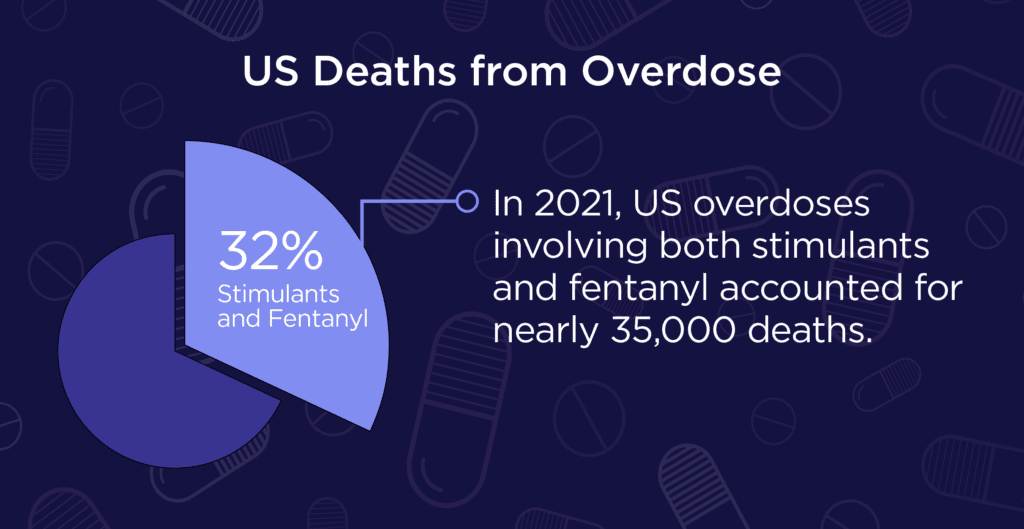
Often, stimulants are used concurrently with fentanyl in an attempt to negate the fatigue associated with opioids. But stimulants increase the body’s need for oxygen while opioids decrease respiration rate, leaving users more susceptible to overdosing. However, it’s important to note that not all users that overdose intended to combine these substances. There have been many reports of people ingesting stimulants that have unknowingly been laced or contaminated with opioids such as fentanyl.
Narcan is now available over-the-counter.
Narcan is available as a nasal spray version of naloxone that, when administered quickly, can reverse an opioid overdose. While commonly carried by paramedics and police officers, this lifesaving medication was previously only available to the general public and advocacy groups through a prescription. But in March of 2023, the U.S. Food and Drug Administration approved Narcan for purchase without a prescription. The landmark decision makes Narcan more widely available and easier to access for people that may not feel comfortable approaching an advocacy group. By September, Narcan had hit the shelves at major retailers such as CVS, Walgreens and Walmart for $45 per dose. The retailers have also made Narcan available online, citing concerns that the stigma attached to Narcan may discourage people from purchasing in person. The price is expected to go down as other products come to market, such as the recently FDA-approved generic version of Narcan and another naloxone-based nasal spray known as RiVive.
The CDC Clinical Practice Guideline for Prescribing Opioids for Pain.
 In 2022, the CDC issued an updated list of recommendations for providers prescribing opioid therapy for pain management. The guidelines stress the importance of prescription drug monitoring programs (PDMP), which are defined as “an electronic database that tracks controlled substance prescriptions.” According to the CDC “PDMPs can help inform point-of-care clinical decision-making to improve patient care and safety. Clinicians should check PDMP data for prescription opioids and other controlled medications patients have received from other clinicians to determine whether a patient is receiving opioid dosages or combinations (e.g., opioids combined with benzodiazepines) that put the patient at high risk for overdose.” At Altera, we’re making it easier to access the PDMP in clinician workflows by providing inline PDMP access directly from the prescription writer.
In 2022, the CDC issued an updated list of recommendations for providers prescribing opioid therapy for pain management. The guidelines stress the importance of prescription drug monitoring programs (PDMP), which are defined as “an electronic database that tracks controlled substance prescriptions.” According to the CDC “PDMPs can help inform point-of-care clinical decision-making to improve patient care and safety. Clinicians should check PDMP data for prescription opioids and other controlled medications patients have received from other clinicians to determine whether a patient is receiving opioid dosages or combinations (e.g., opioids combined with benzodiazepines) that put the patient at high risk for overdose.” At Altera, we’re making it easier to access the PDMP in clinician workflows by providing inline PDMP access directly from the prescription writer.
Other recommendations include how to determine when opioids should be used for pain, how to select the proper opioid and how to decide the duration of treatment. You can read the full set of guidelines here.
Where do we go from here?
The opioid crisis is a multi-faceted problem with no easy answers or solutions. But by staying aware of the latest statistics, treatments and guidelines we can better position ourselves to work with providers, lawmakers and advocacy groups to reach a better future.