Article
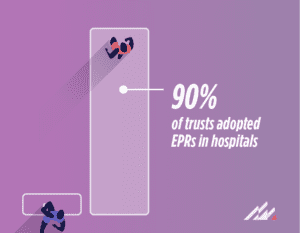
Overcoming barriers: The remaining 10% of NHS trusts and EPR adoption
NHS England recently announced that it has successfully achieved the Government’s target of 90% of trusts adopting electronic patient records (EPRs) in hospitals.[1] However, the journey towards full EPR implementation faces a unique set of challenges for the remaining 10% of NHS trusts, with the anticipated completion date set for 2026.
While this timeline may seem extended, it is crucial to examine the factors contributing to the delay. When I was CDIO at Gloucestershire Hospitals NHS Foundation Trust, we implemented an EPR in a remarkable five months. Now, I question why the final 10% is projected to take several more years. Similarly, success stories—such as at Medway NHS Foundation Trust, which despite intense clinical and operational pressure from COVID-19 achieved EPR deployment in just five months—offer insights into alternative approaches.
As we delve into the reasons behind the delay for the remaining 10% of NHS trusts, several factors come to light as I go into it further.
Budgetary challenges in EPR implementation
One significant hurdle faced by NHS trusts is financial constraints. The cost associated with EPR implementation, including software licensing, training and infrastructure upgrades, can strain the budgets of some trusts. Finding innovative ways to use local budgets or secure funding becomes imperative for these organisations. For example, Worcestershire Acute Hospitals NHS Trust, which was categorised as “Group 0” under the frontline digitisation programme, embarked on its digital transformation journey in March 2023 through the implementation of Altera Digital Health’s Sunrise™. Now, live across all 56 inpatient wards, the ambitious project saw the trust quickly accelerate its digital maturity, developing a highly configured system that is bespoke to the trust’s needs, without national funding support.

With Sunrise, trusts don’t need to rip-and-replace everything they may already have up and running. Concentrating resources on implementing the strategic components that will deliver the greatest value can deliver key functionality and efficiencies faster, instead of going for a one-size-fits-all solution. This is not only more cost-effective, but it also takes a significant pressure off the organisation in terms of deployment effort and change. Additionally, a modular EPR system provides flexibility for future enhancements and integrations, ensuring the solution can evolve with changing requirements.
The crucial role of usability and clinical leadership
Not all NHS trusts are at the same level of organisational readiness for EPR adoption. Factors such as staff training, cultural shifts and change management play a pivotal role in ensuring a smooth transition. The variation in readiness levels among trusts can contribute to the extended timeline for the final 10%. This is why usability and clinical leadership are vital elements for successful EPR implementations.
Intuitive interfaces and workflows enable healthcare professionals to efficiently navigate the system and focus on patient care. Additionally, involving clinicians throughout the design and implementation process ensures that the EPR system aligns with their needs and clinical workflows. Clinicians play a crucial role in driving adoption and acceptance, as their input helps shape the system to best support patient care delivery.
Managing system complexity and integration
The intricacies of healthcare systems, coupled with the need for seamless integration of EPRs with existing technologies, pose considerable challenges. Customisation, interoperability and addressing legacy systems can be time-consuming, contributing to the extended timeline for full adoption.
The flexibility within Sunrise EPR enabled Maidstone and Tunbridge Wells NHS Trust (MTW) to take a phased approach to deployment, enabling a smoother transition. MTW is now one of the top-performing acute hospital trusts in the country and is regularly in the top five for A&E performance in England. It’s also one of the few trusts in the country to have no long waiting patients (those waiting 52 weeks for planned care), and it has delivered the 62-day cancer standard each month for more than three years.
Regulatory compliance and standards
Adherence to regulatory standards and compliance requirements adds another layer of complexity. Navigating the regulatory landscape while ensuring patient data security and privacy can slow down the implementation process.
To maximise the value of EPRs, interoperability and data integration are critical. Healthcare organisations must ensure that their EPR systems can seamlessly exchange information with other healthcare applications and systems. This produces comprehensive patient records, improves care coordination and enhances clinical decision-making. By leveraging standardised data-exchange protocols and open interfaces, NHS trusts can integrate EPRs with existing systems—optimising efficiency and reducing duplicate data entry.
 Strategic prioritisation
Strategic prioritisation
Prioritising EPR adoption amidst other pressing healthcare initiatives requires careful resource allocation. Some trusts may find themselves juggling multiple priorities, affecting the speed at which they can dedicate resources to EPR implementation.
By focusing on core clinical functionality and rationalising speciality-specific configuration and consistent protocolised documentation can not only ensure consistent documentation but also help clinicians follow local guidance. Our Sunrise blueprint configuration provides a launchpad for trusts to accelerate their configuration journeys, saving time in design and development whilst also embedding lessons learned from other NHS sites. This proven methodology has enabled our clients to deploy and adopt key functionality with user input without incurring exorbitant costs or longer timescales to deploy. This approach is open, flexible, works across the entire health IT ecosystem and can be deployed without significant disruption to healthcare services.
While the final 10% of NHS trusts navigate these challenges, it is essential to recognise that each organisation’s journey is unique. Learning from successful case studies like Gloucestershire Hospitals NHS Foundation Trust and Medway NHS Foundation Trust, and addressing specific barriers faced by individual trusts, will be key to expediting the adoption of electronic patient records across the entire healthcare landscape. As we move forward, collaboration, shared insights and innovative solutions will be instrumental in achieving the goal of a fully integrated EPR system, for the benefit of both healthcare providers and patients.
To learn more about how Altera is supporting the NHS, please click here.
[1] https://www.ukauthority.com/articles/nhs-england-hits-national-target-for-epr-roll-out/