Article
Medical tourism, unpacked
Think of the last time you traveled out of the country. Were you taking a much-needed vacation? Visiting family or friends? On business? For a significant number of travelers, “medical tourism” is the driver behind an overseas trip.
Simply put, medical tourism is a term used to describe medical treatment received outside of one’s home country. Medical tourism may not be widely accepted just yet, but it does point to the trend of patients “shopping” for care as healthcare consumers.
If the concept sounds foreign, here are some numbers to put this phenomenon into perspective. In 2017, an estimated 14–16 million people traveled abroad to receive health treatments. And according to the U.S. National Travel and Tourism Office, approximately 1% of Americans who traveled internationally in 2019 did so for medical tourism purposes (though this figure does not include those who crossed the U.S. ̶ Mexico border).
Here are a few things to know about medical tourism today.
 Destinations and procedures
Destinations and procedures
Definitive data on medical tourism is hard to come by as different countries record and track this information differently. Patients Beyond Borders, an organization that researches and vets international options for healthcare, claims the top destinations for medical tourism include Costa Rica, India, Israel, Malaysia, Mexico, Singapore, South Korea, Taiwan, Thailand, Turkey and the U.S.
According the U.S. Centers for Disease Control & Prevention (CDC), Americans seeking medical care abroad frequently travel to Mexico and Canada, as well as countries in the Caribbean, Central America and South America.
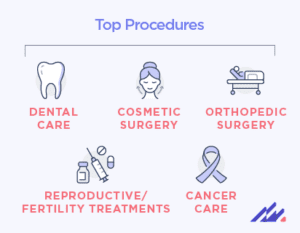
Both organizations say dental care, cosmetic surgery, orthopedic surgery, reproductive/fertility treatments and cancer care are some of the most common procedures medical travelers receive.
Why medical tourism?
It is true that some patients seek medical care abroad as an excuse to see another part of the world and/or recover in a more favorable environment (e.g., trading freezing temperatures for a tropical location). However, there are many other reasons people choose to do so, including:
Cost. One major driver for medical travelers is the total cost of care. Even when factoring in expenses like airfare, lodging and meals, it may be less expensive for a patient to undergo a procedure in another country.
Time. Traveling to another country is unlikely to even be an option for those in need of urgent medical care. That said, patients may opt for treatment outside their home countries to shorten their wait times and reduce time spent in pain or discomfort. For example, data from the Organisation for Economic Cooperation and Development (OECD) indicates that 20% of cataract surgery patients in Denmark waited more than three months from the time of a specialist assessment to surgery. In Australia, more than 50% of cataract patients had to wait three months or more for this procedure.
Culture. The American Hospital Association (AHA) defines cultural competency in healthcare as “the ability of systems to provide care to patients with diverse values, beliefs and behaviors, including the tailoring of healthcare delivery to meet patients’ social, cultural and linguistic needs.” Patients may consider healthcare options outside their country of residence to find providers that speak their native language and/or whose approach to medicine aligns with their culture.
Availability or legality. Patients may look for alternative treatment options if a procedure is not performed where they live or if there are very few providers that offer a particular treatment. Gender-affirming surgery, for instance, is prohibited in several countries, which could necessitate a trip overseas for prospective patients.
 Risk versus reward
Risk versus reward
These and other benefits may be attractive to patients, but they must also be aware of the risks associated with international medical care. First, the CDC cautions that quality of care can differ significantly between countries, as they may have different standards for quality indicators such as licensure, credentialing and accreditation. Another issue to consider is a potential language barrier. If a provider is proficient but not natively fluent in the same language as the patient, communication challenges may arise. Travelers must also bear in mind that antibiotic resistance and infectious diseases may be more prevalent in another country than their own.
Additionally, patients should consider how they may fare after procedures. Air travel post-surgery can increase the risk of blood clots; patients receiving chest, abdominal and facial cosmetic procedures should wait at least 10 days before flying home. Finally, patients should identify options for follow-up care in case they experience complications once they are back at home to ensure there is continuity of care.
Healthcare decisions are very personal decisions. That is evidenced through a whole host of patient preferences, including the facility—and country—they choose for their care needs. As medicine and travel become more accessible for more people around the world, it will be fascinating to see how the healthcare industry evolves in response.
Learn more about medical tourism here.

 Risk versus reward
Risk versus reward