Article
How two hospitals leverage Allscripts Sunrise™ to improve sepsis outcomes
* This content was originally published prior to N. Harris Computer Corporation’s 2022 acquisition of the Allscripts Hospital and Large Physician Practice business segment. Our business is now known as Altera Digital Health.
Sepsis, a life-threatening response of the body to infection, accounts for approximately 6% of admissions to U.S. hospitals, and it is the number one cause of hospital death. [1] Additionally, sepsis is the number one hospital cost with more than $24 billion spent per year in the United States. [2]
Because unrecognized sepsis can be rapidly fatal, one key to improving sepsis outcomes is early recognition and prompt treatment of the condition. Symptoms and signs of sepsis are often non-specific and may mimic other conditions and, in some cases, may be very subtle, particularly in older patients.
The electronic health record (EHR) is a highly effective tool to help in early identification and treatment of sepsis. Key components within the EHR include:
- Sepsis early warning system
- Sepsis order sets using evidence-based content to standardize care and reduce variation
- Real-time monitoring for those with suspected sepsis to identify care gaps
- Retrospective reporting to measure sepsis care processes and outcomes across a population
Two Sunrise clients have effectively used early warning systems within the EHR.
In 2016, University Hospitals implemented an early warning system that leveraged medical logic module (MLM) functionality, along with sepsis order sets and real-time monitoring, resulting in a 30% reduction in sepsis mortality, saving an estimated 206 lives. A sophisticated statistical analysis concluded that this early warning MLM was directly responsible for these favorable outcomes.
MLMs function in the background and are “always on and always listening” for triggering(s) event on which to act. The MLM used for early identification of possible sepsis continuously “listens” for certain features, including newly entered vital signs (e.g., heart rate, temperature) and lab results (e.g., white blood cell count) reported in Sunrise. The new data is immediately used to calculate a sepsis risk score, and when a pre-determined threshold of risk is reached, end users are immediately notified. This crucial communication step can be an alert within the EHR or a message sent to a pager or texted to a smart phone to specific clinician(s) or a group, such as a rapid response team.
Once suspected sepsis has been validated, next steps include rapid implementation of a sepsis care bundle, including obtaining lab test results and administration of antibiotics, and as indicated, intravenous fluids and vasopressors and possibly transfer to the ICU. A patient with suspected sepsis can be placed on an Advanced Visit List, which serves as a real-time care monitoring tool to track care bundle elements and identify care gaps.
In 2017, Carson Tahoe Health, another Sunrise client, used the approach taken by University Hospitals as part of its sepsis quality improvement initiative. This client with roughly 200 beds and a relatively small IT team, implemented the solution with few changes, which included adjusting sepsis order set antibiotic options reflecting local antibiotic resistance patterns and formulary availability.
The sepsis solution was implemented in September of 2017, and over time Carson Tahoe Health realized favorable outcomes in its sepsis patients. Statistically significant changes over time included:
- Reduced mortality
- Shorter length of stay
- Inverse correlation between early identification and mortality
- Inverse correlation between sepsis order set use and length of stay
- Higher net revenue

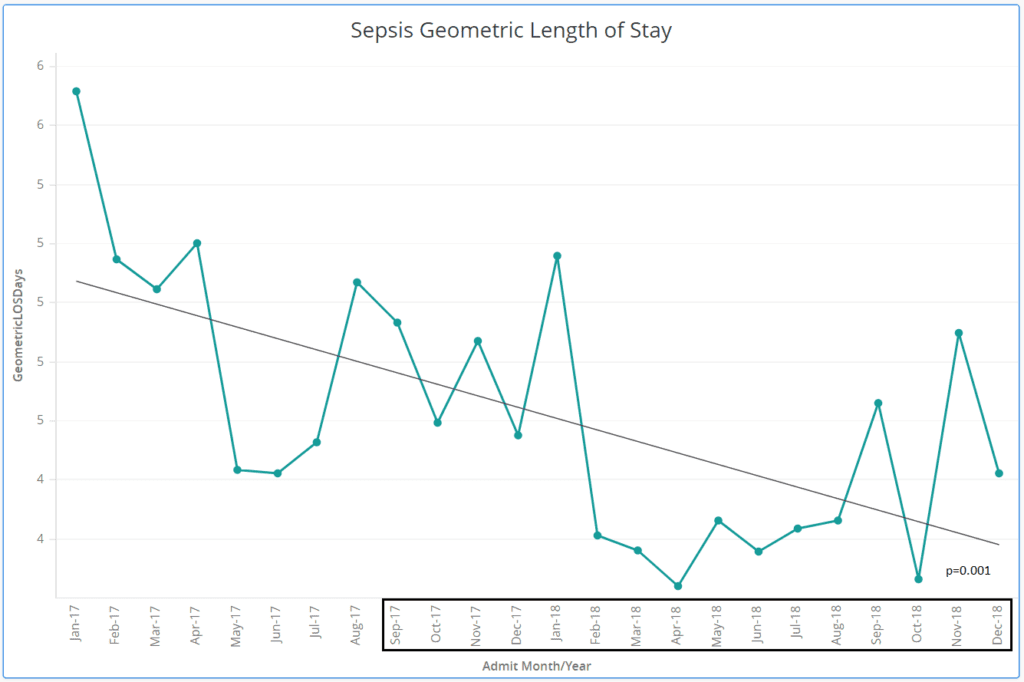
In addition, Carson Tahoe Health also realized improved financial impact for three sepsis DRGs, which was attributed to a shorter length of stay. Patients identified earlier likely avoided prolonged care needed for those with more severe illness.

As noted above, signs and symptoms of sepsis often mimic other conditions. One challenge using sepsis early warning systems is balancing identification of patients with sepsis (true positive) and avoiding mis-identifying those without the condition (false positive). Over alerting may result in alerts being ignored (alert fatigue) and negate benefit from the alert. Some clients increase the alert firing threshold from two to three parameters to reduce over alerting.
With the increasing use of machine learning tools in healthcare, sepsis prediction models will be more rapidly developed and hopefully more accurate in their predictive capability.
While some studies suggest stabilization of sepsis incidence others show an increase [2]. Regardless, sepsis remains a significant threat to patients and requires active surveillance to identify early and systems in place, facilitated by Sunrise to rapidly treat and monitor to achieve better clinical and financial outcomes.
References
- Sepsis syndromes in adults: Epidemiology, definitions, clinical presentation, diagnosis, and prognosis, UpToDate, Literature review current through: Feb 2019. | This topic last updated: Oct 01, 2018
- Educating the Public About Sepsis, Centers for Disease Control