Article
Challenge accepted: Top concerns for provider practices in 2023
Over the last decade or so, we have seen increases in acquisitions of independent physician practices by hospital groups, private equity firms and other corporations. And according to the American Medical Association (AMA), 54% of physicians worked in physician-owned practices in 2018. In 2021, that number decreased to 49%.
Although healthcare organizations of all sizes share some of the same challenges, they can affect private practices in unique ways. Here are some of the top issues practices are facing in the year ahead.
Personnel problems
It may come as no surprise that staffing issues are a major concern for independent practices. A recent survey by the Medical Group Management Association (MGMA) found that 58% of medical practices say it will be their biggest challenge in 2023. (This was the top concern in the previous year’s survey, as well.) Healthcare organizations around the world have felt the squeeze of staffing shortages for years—even before the pandemic—but it may feel especially pronounced at a practice.
Think of the hiring process as an example. A large health system may have multiple teams of employees focused solely on writing and posting job descriptions, conducting outreach, vetting qualified candidates, scheduling interviews and managing contract negotiations. At an independent practice, these duties might be shared among staff members that have other core responsibilities, from accounting to providing patient care.
Conversely, consider how the departure of a single staff member can affect a healthcare organization. At a large hospital, this might mean distributing the former employee’s tasks among other team members until a new person is hired. However, the loss of institutional knowledge can have a much larger impact at an independent practice, where perhaps only one person manages prior authorizations or claims submissions.
And even when a practice has adequate staffing across clinical, financial and operational roles, challenges often remain. With a smaller staff, it is more difficult to offer flexible scheduling options like early morning and late afternoon/early evening appointments. While practices may be inclined to provide care that fits into patients’ busy schedules, they must be able to find and retain employees that are willing to work outside “normal” business hours (whereas a large hospital system might rotate who works during less desirable hours more easily).
The post-pandemic environment
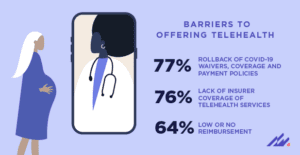 We are now nearly three full years into the pandemic. While many aspects of our everyday lives have returned to some version of normal, the healthcare system must continue evolving as the risk of COVID-19 remains. One of the biggest shifts we’ve seen in light of the pandemic is the rise in telehealth. Although many providers appreciate the convenience, accessibility and flexibility that telehealth offers, uncertainty around payment models persists. In a survey of physicians from the AMA, the most frequently reported barriers to offering telehealth were the rollback of COVID-19 waivers, coverage and payment policies (77%), lack of insurer coverage of telehealth services (76%) and low or no reimbursement (64%).
We are now nearly three full years into the pandemic. While many aspects of our everyday lives have returned to some version of normal, the healthcare system must continue evolving as the risk of COVID-19 remains. One of the biggest shifts we’ve seen in light of the pandemic is the rise in telehealth. Although many providers appreciate the convenience, accessibility and flexibility that telehealth offers, uncertainty around payment models persists. In a survey of physicians from the AMA, the most frequently reported barriers to offering telehealth were the rollback of COVID-19 waivers, coverage and payment policies (77%), lack of insurer coverage of telehealth services (76%) and low or no reimbursement (64%).
The murkiness surrounding telehealth’s future highlights a broader challenge for providers in the ambulatory space: Reimbursement for outpatient services is not stable or predictable. This makes it difficult for practice owners to forecast their financial performance. And as non-traditional healthcare startups and technology companies push further into the ambulatory market, independent practices will need to make investments that keep their practices competitive and appeal to patients.
In addition to these reimbursement-related obstacles, practices are also contending with ongoing disruptions in the global medical supply chain. In one recent survey of healthcare industry professionals, 57% of respondents said they could recall a time when a physician did not have a product required for a procedure. Supply chain issues affect all types of organizations, but an independent practice likely does not have the same negotiating power that a large healthcare system can leverage to maintain adequate supply levels.
While these issues pose challenges for provider practices, they are not insurmountable. With the right tools and technology partners, practices can continue delivering high-quality care, embrace innovation and remain independent. Learn how the TouchWorks® EHR can support your practice’s needs here.












